Resource Details
Resource Format
Categories
Share:
In the past, some clinicians believed autistic people do not feel pain the way neurotypical people do, which was to say they thought that people who could not verbally communicate about their pain not feeling pain. We now know this isn’t true. Autistic people often find that when they feel pain they can’t explain it or locate the source of it as easily as most neurotypical people can.
Some autistic people may be more sensitive to pain than their neurotypical peers. This can be especially true for girls and women who have autism. This is why talking about pain is one of the most critical conversations to have with a new provider, and it should happen before the first physical exam.
Behaviors that may indicate pain in non-verbal adults
It’s sometimes hard to distinguish between behaviors that indicate pain and those that seek to communicate another problem. Some of the common pain related behaviors are:
Aggression
Running, pacing, bolting
Jumping, stomping, thrashing
Self-injury, sometimes, but not always at the source of the pain (such as banging/hitting head when having GI pain)
Subtle or strong pinching or grabbing body part that source of pain
Sudden, exaggerated repetitive actions, like hand flapping or throat scratching
Twisting or irregular motions/positions to make accommodations for discomfort
Screaming
Ingestion (e.g. overeating, quickly ingesting food and drink, food avoidance, vomiting, mouthing or eating non-food items)
Crying
Withdraws or becomes very still
Checklist for talking to a clinician about pain
It can be helpful to carry a list of pain-related concern to appointments. It might include:
It hurts when people touch me without asking first.
The thought of feeling pain makes me very nervous.
If something will cause pain, please tell me ahead of time.
If something will cause pain, please give me medicine or treatment to help it hurt less.
Pain scares me.
I don’t like needles and need to know if there will be shots or blood draws that might be painful
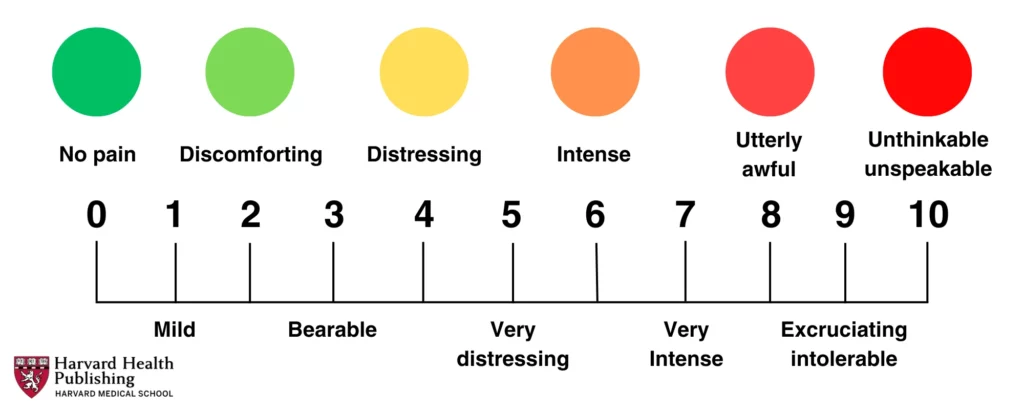
Using a Pain Scale
If a medical appointment involves addressing pain as a problem or symptom, it may be helpful to use a tool known as a pain scale. Pain scales give patients a way to self-report their pain in a way that helps clinicians make an accurate evaluation and diagnosis of underlying health issues.
There are several kinds of pain scales:
One type of pain scale involves patients assigning a number between 1 and 10 to . One would be “no pain,” and 10 would be the worst pain imaginable.
A non-verbal pain scale for adults may also be used to help communicate about and identify the source and severity of pain. Karen Turner, OT and Patient Navigator at Massachusetts General Hospital, explains:

Karen Turner, OT, is a Patient navigator at the Massachusetts General Hospital in Boston
The Massachusetts General Hospital Patient Accommodations Care Plan is useful communication tool that allows patients and families to document important conditions and behaviors that clinicians should know, including pain.
More information
Neuroscience News on People with Autism Experience Pain at a Higher Intensity
Recent research on autism and pain in adults.
DOWNLOAD
A detailed form that can be used to outline special considerations for making health care environments more manageable and comfortable for autistic adults

Additional Resources