Respect in Health Care for Autistic Adults
Helping adults to navigate the health care system as well as communicate and advocate for high-quality care in collaboration with their clinical providers.
Header image adapted from original artwork by Billy Megargel titled: Cross Sections (for more information see About Us)
Easy access to essential health information
We've developed a toolkit that connects to important health resources relevant to all stages of adulthood
Make important health decisions easier
Our Autism Health Care Toolkit supports caregivers and advocates in exploring vetted and actionable information around important health needs for autistic adults.
Training for providers
Advocates and caregivers can share with existing providers Harvard Medical School’s latest clinician course that’s geared toward educating health providers on supporting autistic adults.

Support for all transitions
Help for autistic adults and caregivers across the lifespan
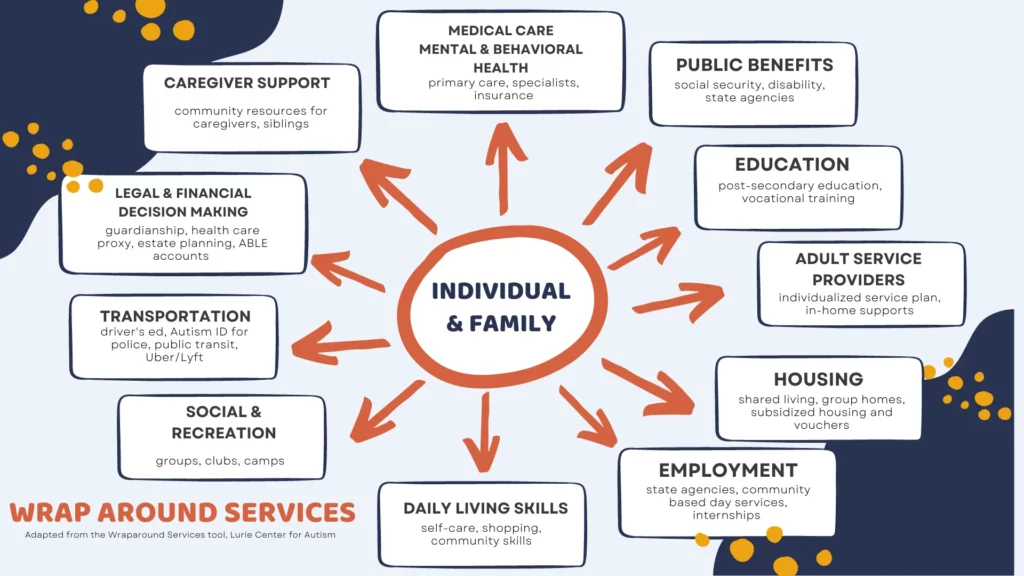
Explore and engage with health resources that support adults transitioning through ages and stages of life.

Young Adults
The transition years from school to adult programs set the stage for the a full life, and health care choices are a key part of that.

Midlife Adults

Older Adults

Young Adults
The transition years from school to adult programs set the stage for the a full life, and health care choices are a key part of that.

Midlife Adults

Older Adults
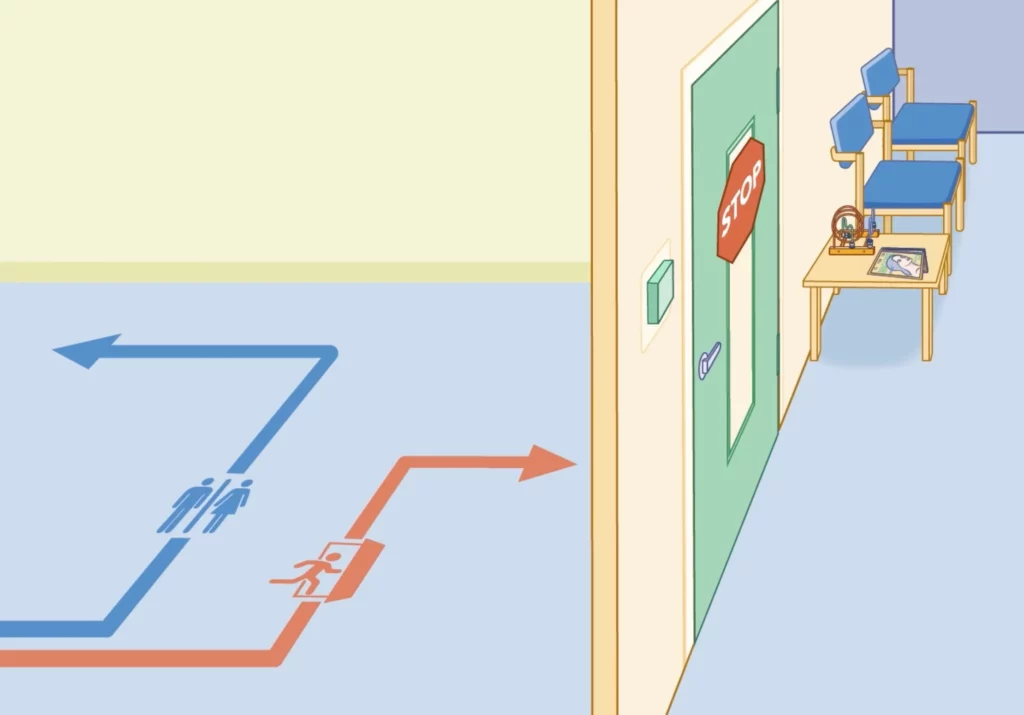
Manageable moments
Understanding and improving the adult health care experience
Finding the people and places that meet each person’s needs


words matter
The Language of Autism
We understand that how we talk about autism matters. Our intent is always to incorporate language that is accessible, inclusive, and reflective of the priorities of the autistic community.

Dr. Tim Buie on the important role caregivers play on the medical team
The clinician-caregiver partnership is vital to successful health care experiences.
Empowering advice on caregivers and patients as experts.
